Introduction:
In recent years, the rapid advancement of health technology, or HealthTech, has emerged as a transformative force within the global healthcare landscape. From telemedicine and wearable devices to artificial intelligence-driven diagnostics and electronic health records, these innovations are poised to redefine healthcare delivery, accessibility, and quality. However, as HealthTech continues to proliferate, a critical examination of its impact on global health disparities is warranted. The integration of technology into healthcare systems has the potential to bridge gaps in access and treatment, particularly in underserved populations. Conversely, it also raises concerns regarding the equitable distribution of resources and the risk of exacerbating existing inequalities. This article seeks to explore the dual-edged sword of HealthTech through a comprehensive analysis of its influence on health disparities across various regions, particularly in low- and middle-income countries. By scrutinizing case studies and empirical data, we aim to identify key drivers, barriers, and best practices that may inform policy and innovation strategies to ensure that the promise of HealthTech contributes meaningfully to the goal of health equity on a global scale.
Table of Contents
- Evaluating the Impact of Health Technology on Vulnerable Populations
- Barriers to Access: Analyzing Inequities in HealthTech Implementation
- Metrics for Success: Measuring HealthTech Outcomes in Diverse Environments
- Strategic Initiatives: Recommendations for Bridging Health Disparities through Technology
- In Summary
Evaluating the Impact of Health Technology on Vulnerable Populations
The integration of health technology into healthcare systems presents a unique opportunity to address the multifaceted challenges faced by vulnerable populations. However, to effectively leverage these innovations, it is crucial to analyze how technology can either bridge or exacerbate existing health disparities. Factors to consider include:
- Accessibility: Are health technologies designed with the needs of all communities in mind?
- Training: Do healthcare providers have adequate training to implement tech solutions in underserved areas?
- Infrastructure: Is the necessary infrastructure, such as internet access, available to those in need?
In examining successful case studies, it becomes evident that the design and distribution of health technology must prioritize inclusivity. For example, mobile health applications in low-income regions have shown promise by:
- Enhancing communication: Facilitating consistent communication between patients and providers.
- Streamlining access: Providing on-demand access to healthcare resources and information.
- Promoting preventative care: Encouraging health monitoring and early intervention strategies.
| HealthTech Initiative | Target Population | Impact |
|---|---|---|
| Telemedicine Access | Rural Communities | Decreased travel time for healthcare |
| Mobile Health Apps | Low-Income Families | Improved health literacy |
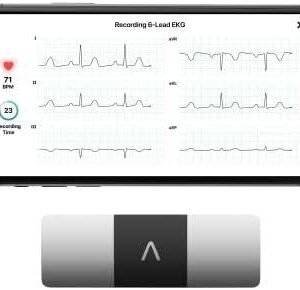
| Wearable Devices | Chronic Disease Patients | Better management of health conditions |
Barriers to Access: Analyzing Inequities in HealthTech Implementation
The advent of HealthTech holds immense promise for transforming healthcare delivery, yet its implementation often encounters significant barriers that contribute to existing inequities. Technological literacy remains a critical hurdle, particularly in underserved populations where access to education and training is limited. Without adequate support and resources, these communities are at risk of further marginalization as they struggle to integrate advanced health solutions into their daily lives. Additionally, the digital divide exacerbates disparities, as inconsistent internet access and lack of devices prevent equitable engagement with HealthTech innovations, reducing their impact where they are needed most.
Furthermore, cultural attitudes towards technology can impede the adoption of health solutions. In regions where traditional practices dominate, there may be skepticism towards digitally-mediated care, leading to resistance against interventions that prioritize technological over human interaction. Another critical aspect is the fragmentation of healthcare systems, where siloed information and lack of interoperability among platforms prevent seamless patient care. This can create unnecessary barriers for patients trying to navigate diverse health services. Addressing these multifaceted challenges requires a concerted effort from stakeholders across sectors, including policymakers, technologists, and community leaders.
Metrics for Success: Measuring HealthTech Outcomes in Diverse Environments
Evaluating the impact of HealthTech initiatives requires a multifaceted approach that accounts for a variety of factors influencing healthcare outcomes across different populations. Key metrics can provide insights into effectiveness, accessibility, and user adoption, contributing to a holistic understanding of HealthTech’s role in addressing disparities. Important performance indicators include:
- Patient Outcomes: Tracking changes in health status, including mortality and morbidity rates.
- Utilization Rates: Analyzing the frequency of HealthTech tool adoption among various demographic groups.
- Cost-Effectiveness: Measuring dollar savings from using technology versus traditional methods.
- User Satisfaction: Gathering feedback through surveys and user experience studies.
Moreover, integrating data from diverse environments enhances the robustness of findings. By stratifying data, stakeholders can identify disparities specific to various populations. For example, a comparison of telehealth services in urban versus rural settings can reveal critical accessibility challenges. To summarize these insights effectively, the table below illustrates potential disparities in HealthTech usage:
| Population Segment | Telehealth Utilization (%) | Reported Barriers |
|---|---|---|
| Urban Elders | 70% | Technology literacy |
| Rural Residents | 45% | Internet access |
| Low-Income Families | 60% | Cost of services |
Strategic Initiatives: Recommendations for Bridging Health Disparities through Technology
To effectively bridge health disparities through technology, it is crucial to leverage tools that enhance access and quality of care for underserved populations. Telehealth services can be expanded to facilitate remote consultations, allowing individuals in rural or low-income urban areas to connect with healthcare providers without the barriers of travel. Additionally, tailored mobile health applications can empower users by providing health education, medication reminders, and monitoring tools that address specific challenges faced by diverse communities. Emphasizing user-friendly interfaces and multilingual options can significantly improve engagement and usability among diverse populations.
Collaboration between public health organizations, technology developers, and community leaders is essential to create sustainable initiatives. Funding should be directed towards innovative pilot programs that assess the effectiveness of technology in bridging gaps in health equity. These initiatives should focus on:
- Data Collection: Gathering demographic data to identify and target at-risk groups.
- Feedback Mechanisms: Implementing channels for user feedback to continuously improve services.
- Awareness Campaigns: Promoting available resources through community engagement.
By focusing on these strategic pillars, we can create a more inclusive healthcare ecosystem that minimizes disparities and enhances overall community health outcomes.
In Summary
the intersection of HealthTech and global health disparities presents both significant opportunities and challenges. As we have explored, innovative technologies have the potential to address critical gaps in healthcare access, quality, and delivery, particularly in underrepresented and underserved populations. However, the effective implementation of these technologies necessitates a nuanced understanding of local contexts and the socio-economic determinants that shape health outcomes.
While advancements such as telemedicine, mobile health applications, and artificial intelligence can enhance healthcare delivery and decision-making, it is imperative that stakeholders remain vigilant in assessing their impact on equitable health access. Continuous monitoring and evaluation will be crucial in ensuring that HealthTech serves as a tool for empowerment rather than exacerbation of existing disparities.
Moving forward, interdisciplinary collaboration among technologists, healthcare providers, policymakers, and communities will be essential in harnessing the full potential of HealthTech. By prioritizing inclusivity and ethical considerations in technology design and deployment, we can work towards a more equitable health landscape, ultimately fulfilling the promise of improved health outcomes for all populations, regardless of their geographic or socio-economic circumstances.
As we stand at the forefront of this technological revolution, it is our collective responsibility to ensure that the benefits of HealthTech are shared widely and that disparities in health equity are not only acknowledged but actively addressed.